This is the first story in a partnership between the Wellcome Trust and WikiTribune to publish evidence-based science reports which are open to editing and discussion from the WikiTribune community.
For eye specialist Francesca Cordeiro, eyes are a window onto people’s brains – a window that looks onto the prospect of stopping and even reversing blinding conditions.
Ten seconds after her team injects their invention into a patient’s hands, the specialists look through their patient’s pupils to see a glowing dye start to appear inside their eyes. The dye is linked to a protein molecule found naturally in our bodies, annexin, which attaches to dying cells. An hour after injection, the opthalmologists start taking pictures showing whether annexin has bound to any sick cells in their eyes.
“Being able to look directly onto microscopic structures is incredible,” says Cordeiro, who works at both University College London (UCL) and Imperial College London in the UK.
The vulnerability of our eyes, two delicate structures filled with fluid, also makes them much easier to study and potentially repair. They are easy to get at, as they’re not hidden inside the body, and our pupils are transparent, so we can see inside. They’re also “immunoprivileged,” meaning that if we put foreign objects into them, the immune system won’t immediately mobilize to destroy the objects.
These benefits mean that scientists are making exciting progress with studying and diagnosing disease – such as with Cordeiro’s test, called DARC (Detection of apoptosing retinal cells). They are also tackling blindness through gene therapy, stem cells, and tiny light-detecting microchips. And these breakthroughs could all have much wider benefits in the future, helping develop new treatments for illnesses in parts of the body that are much harder to access.
Under pressure
It was frustration with the potentially-blinding condition glaucoma that drove Cordeiro to develop the DARC test. Glaucoma results from damage to the optic nerve connecting our eyes and brains. It affects 60 million people worldwide, blinding one in ten. And although we don’t understand its cause well, we do know that pressure in the eye plays a role.
“What I think is a heart-sink moment for any doctor is that you have the patient in front of you, you’ve thrown everything at them,” Cordeiro says. “There’s nothing more you can do to lower their eye pressure, and yet they carry on losing vision. So, one thing that inspired me is the idea that we can see whether drugs that we are giving are working effectively earlier.”
With current glaucoma tests, patients have already lost up to half of their nerve cells before a defect is identified. In 2003, the UK’s Guide Dogs for the Blind Association estimated that if 10 percent of glaucoma cases were picked up earlier through screening, the government would save up to £1 billion a year in non-treatment costs alone. With the world’s population having aged since then, more people are getting glaucoma, and more of them are going blind.
With DARC, Cordeiro and her team aim to spot dying cells in the eye – the earliest signs of glaucoma – so sufferers can get treatment before they start losing their sight. In 2015 and 2016, they ran a phase I trial, whose main function is usually to check safety in a small number patients. That showed that DARC could count sick cells in the retina at the backs of the eyes of 16 patients without serious side-effects.
They have since run phase II trials, which are larger and start exploring how good a treatment is and how best to give it. This time, in 120 people, Cordeiro and her colleagues have moved beyond glaucoma to look at different blinding illnesses and other areas where the window in the eye offers illumination. One surprising opportunity is related to Alzheimer’s disease, where evidence from animals suggests retina cells may offer an early warning that people have it.
Cordeiro’s team also IS hoping that DARC could one day help other fronts in the battle against blindness, including enabling revolutionary gene therapy and stem cell-based treatments. And one of the nearest prospects for using gene therapy is to treat an inherited blindness condition called choroideremia. (Link is to U.S. National Library of Medicine).
Gene swap
People with choroideremia typically begin to lose their sight in early childhood, and progressively worsen. The ailment is caused by a mutation in a gene on the X chromosome. That means that it usually affects males, since females have a second X chromosome that can compensate. The mutation leads to the destruction of the light-detecting rods and cones in affected people’s retinas, affecting around 1-in-50,000 people.
Gene therapy – long heralded as a way of tackling genetic disease – is now helping people with choroideremia thanks to the University of Oxford’s Robert MacLaren and his team. They have been devising a way to insert a working copy of the mutated gene into retina cells.
It’s difficult to get genes safely into the cells where they need to be, an issue researchers developing gene therapy treatments have been wrestling with for decades. The usual approach is to insert the gene into the empty outer shell of a virus, but in some treatments that has caused seriously problematic immune responses in patients. MacLaren’s team therefore uses adeno-associated virus (AAV) – a small, simple virus that elicits only a weak immune response and does not cause human disease.
So far, MacLaren’s team has published promising results from treating six choroideremia patients. They lifted the retina in one of each patient’s eyes and injected the gene therapy into the space underneath, leaving the other untreated as a comparison. Some participants’ vision improved, including being able to detect more light, and to read better. All five given a high dose could read with the treated eye better than, or the same, as the untreated eye after three-and-a-half years. “Patients who gained vision in our gene therapy trials have maintained the vision gain for as long as we have been following them,” MacLaren said.
Integration issues
The treatment is now being commercialized by the company MacLaren founded, Nightstar Therapeutics. Nightstar is intending to take it into phase III clinical trials, the usually-large studies designed to provide conclusive evidence of whether a treatment works, in early 2018. Other gene-therapy treatments for blindness are further advanced, and one looks set to get the OK to be prescribed commercially in 2018.
“We will see the first regulatory approvals soon and suddenly, diseases which were considered incurable causes of blindness when I started out will now have a licensed treatment available,” MacLaren says. “This is an incredible success.”
Yet such apparently-successful virus-delivered treatments may stop working, suggests University College London (UCL) ophthalmologist Mariya Moosajee, meaning patients might need another dose. That dose might then cause an immune reaction because the body has been sensitized to the virus.
“And because it’s a virus it integrates within our DNA and has the potential to introduce mutations that can lead to cancer,” Moosajee adds. “So we have to be cautious.”
The solution could be gene therapy without viruses. Moosajee is working on this idea with Hans Lipps at the University of Witten/Herdecke in Germany and Richard Harbottle at the German Cancer Research Centre in Heidelberg. They use a piece of human DNA called a “scaffold matrix attachment region” that helps our genes fold up properly. Delivered as a gene therapy into cells, it sits next to existing DNA, without integrating into it.
“Because it’s made up of human components it doesn’t evoke an immune response and, as it doesn’t integrate into DNA, you’re less likely to introduce mutations,” she says. But what if, rather than trying to repair faulty, damaged or dying cells in the eye this way, we could just replace them?
Cell yourself
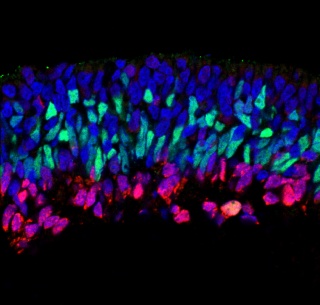
Moosajee and her team are testing one approach to replacing eye cells, editing out blindness-causing mutations from skin cells, and then – amazingly – growing them to become eye cells. They take two batches of patients’ skin cells, and convince them to revert into stem cells. The UCL team can then grow the stem cells into model eyes, using a technique called CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats – link to Broad Institute) to remove harmful, disease-causing mutations from one of the two batches. Their hope is that they’ll see normal eye cells in the edited batch.
Although the research is currently at a very early stage, if this technique works, the edited cells could be implanted into a patient’s eye. Because they’re the patient’s own cells, the risk of serious immune reactions is low, Moosajee says.
Stem cell implants – without CRISPR corrections – are closer to reality at the California Project to Cure Blindness. Rather than genetic defects, the project is targeting age-related macular degeneration (AMD), where cells in the retina die in older people. The project team, involving various California universities and hospitals, is growing the stem cells on a plastic scaffold, explains Dennis Clegg from the University of California, Santa Barbara.
“It’s like a contact lens material, a 3 mm x 6 mm piece of plastic, coated with cells,” Clegg says. Surgeons can then implant these into patients’ eyes.
Having checked their safety – particularly the cancer risk – in rats and pigs, in 2016 the California Project started a phase I/IIa clinical trial to test their safety in 20 people blinded by AMD.
“The patients…are my heroes..They’re willing to try this method that has never been done in humans,” Dennis Clegg – UC-Santa Barbara
‘Opthalmonauts’
“The patients in this phase I trial are my heroes,” Clegg says. “They are like the first astronauts into space. They’re willing to try this method that has never been done in humans. It’s very altruistic and brave in that it will inform us how to approach this and hopefully help patients in the future.”
The California Project’s method may turn out not to work, Clegg admits.
“There are going to be successes and failures in clinical trials,” he says. “It’s really important to understand that a lot of treatments don’t make it. Even if they fail we still learn something. That knowledge will help us go forward.” He adds that there are ‘about a dozen different groups’ looking to treat AMD with stem cells, and so the chances are good that at least one of them will succeed.
MacLaren is among the others working on stem cells for AMD, but he has concerns about too many groups rushing into human trials.
“This is a very exciting future area of regenerative medicine that could reverse blindness,” he says. “I think it is a bit like gene therapy was 20 years ago – more lab work needed but huge potential. We do however need to avoid the same mistakes that were made in gene therapy. We need to avoid forcing stem-cell therapy into clinical trials before we understand the basic mechanisms. We need a better understanding of how cells might reconnect in the retina.”
Bionic eyes
If patients do lose their sight, another technology altogether might be the best option: bionic eyes. Over the last five years, MacLaren has implanted 12 bionic eyes developed by the German engineering company Retina Implant AG into patients. The collaboration has delivered “excellent results,” he says, with “sustained function of the chip and visual benefits to the patients.” MacLaren now hopes to get approval from the UK’s National Health Service to use the implants routinely “in a select group of patients in the near future.”
“We’ll learn a huge amount in the eye that we can then apply elsewhere…particularly in the brain.” – Robert MacLaren – University of Oxford
The most important broader lessons from new technologies developed in the eye are for gene therapy, MacLaren stresses.
“I think we can learn a huge amount in the eye about dose, duration and effects of gene therapy in an advanced way that is simply not possible elsewhere in the body,” he says. That’s in part thanks to the windows provided by our eyes’ pupils allowing researchers to “actually look at the cells that have been exposed to the virus and measure the effects with a high level of precision.”
Links to neurological conditions like Alzheimer’s and Parkinson’s disease are especially promising, adds MacLaren. “We will learn a huge amount in the eye that we can then apply elsewhere to other diseases, particularly in the brain,” he stresses.
By Andy Extance and 3 collaborators